September 13, 2025
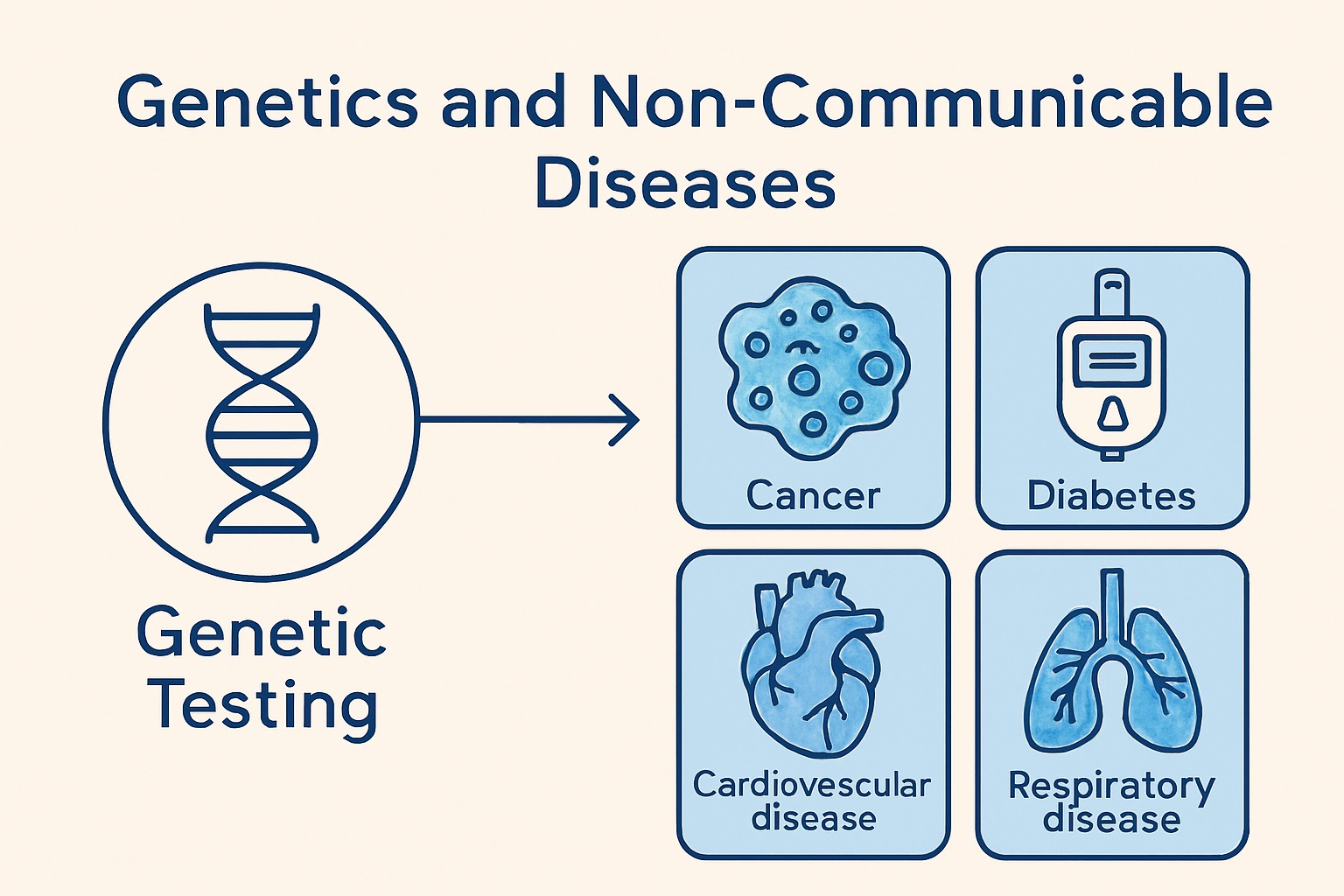
Genetics and the Silent Burden of Non-Communicable Diseases
Non-communicable diseases (NCDs)—including cancers, diabetes, cardiovascular diseases, kidney disorders, and chronic lung and liver conditions—are not caused by infectious agents and often develop gradually over time, earning the label “chronic.” Increasingly, research shows that genetic information plays a significant role in both the development and progression of NCDs, either through primary involvement, where genetic mutations directly initiate or predispose individuals to disease, or secondary involvement, where chronic disease progression influences gene expression or function. In cancer, genetic testing is now routine for identifying hereditary syndromes, including Lynch syndrome (MLH1, MSH2, MSH6, PMS2, EPCAM), Hereditary Breast and Ovarian Cancer (BRCA1, BRCA2), Cowden syndrome (PTEN), and VHL syndrome (VHL), with targeted therapies and immunotherapies increasingly relying on genetic profiling before treatment. Cardiovascular conditions also show strong genetic links, such as Familial Hypercholesterolemia (LDLR, APOB, PCSK9, ApoE), heart failure (HCM & DCM; MYH7, TNNT2, TNNI3), and congenital heart disease with over 400 implicated genes. Diabetes has genetic components as well, with Type 1 Diabetes linked to autoimmune-related genes (HLA-DQA1, HLA-DQB1, HLA-DRB1) and Type 2 Diabetes involving multiple genes affecting insulin resistance and beta-cell function. Lung diseases also have genetic associations, including cystic fibrosis (CFTR) and idiopathic pulmonary fibrosis (ASPN, CDH2, COL1A1, COL1A2, COL3A1, CTSK, MMP1, MMP7, POSTN, SPP1). Integrating genetic insights into disease management is no longer optional—it is essential.